Our commitment to community health
Together with community partners, we’re building a holistic and equitable healthcare system designed to improve everyone’s health and wellness.
Clinical care can diagnose, treat, and often cure diseases, but we recognize health is more than that. Social and economic factors like systemic racism, trauma, access to healthy food, housing, and jobs impact more than 50% of people’s well-being.
Our community health programs are focused on making systemic changes and improving a wide range of issues that have deep and long-lasting impacts on how we live, work, and play.
Our goals
What is a community health needs assessment?
A community health needs assessment (CHNA) identifies both assets and resources that support healthy communities, as well as health challenges and disparities.
The assessments gather data and community input on a wide range of health issues including:
- the health of community members (demographic characteristics, births, deaths, chronic conditions, communicable diseases, mental health),
- health behaviors (substance use, physical activity, nutrition),
- accessible and affordable health care, including preventive health such as health care screenings, immunizations, and dental care, and
- healthy and safe environments, and social and economic factors that influence health (education and employment, affordable housing, social support).
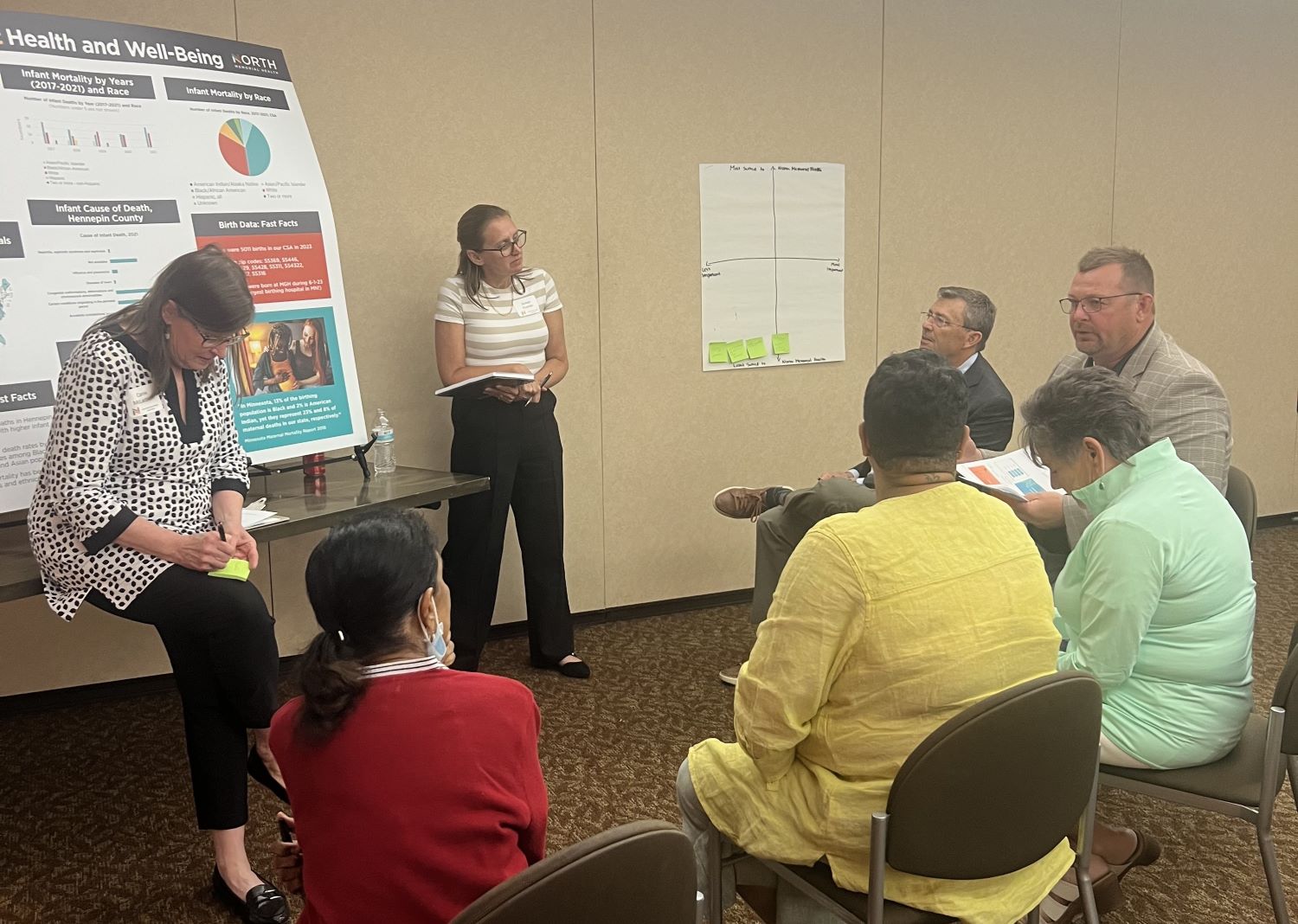
Data comes from both primary and secondary data sources. Secondary sources include local health surveys that gather information on the health of youths and adults in the community such as the Minnesota Student Survey and Hennepin County’s SHAPE survey. Primary data collection occurs by intentionally engaging with community members and organizations to identify and understand significant health needs in the community and seek input on addressing gaps and barriers so community members can lead healthy lives.
Working closely with the hospitals’ Community Engagement Advisory Team (CEAT), data from all these sources is reviewed and priority health issues are selected for action. Partnering with the CEAT, community partners, and community members, a community health implementation plan is developed that outlines strategies for addressing the priority health issues.
2025 community health needs assessment
Both North – Robbinsdale Hospital and North – Maple Grove Hospital routinely conduct Community Health Needs Assessments, working closely with partners in our community to help us identify our community health priorities.
The top three priorities we identified for 2026-2028 are:
- Establish Care with a Primary Care Provider and/or Health Clinic
- Understand and Navigate the Healthcare System
- Prevent, Detect, and Manage Chronic Diseases
We are committed to focusing on and improving our community’s health in these areas.
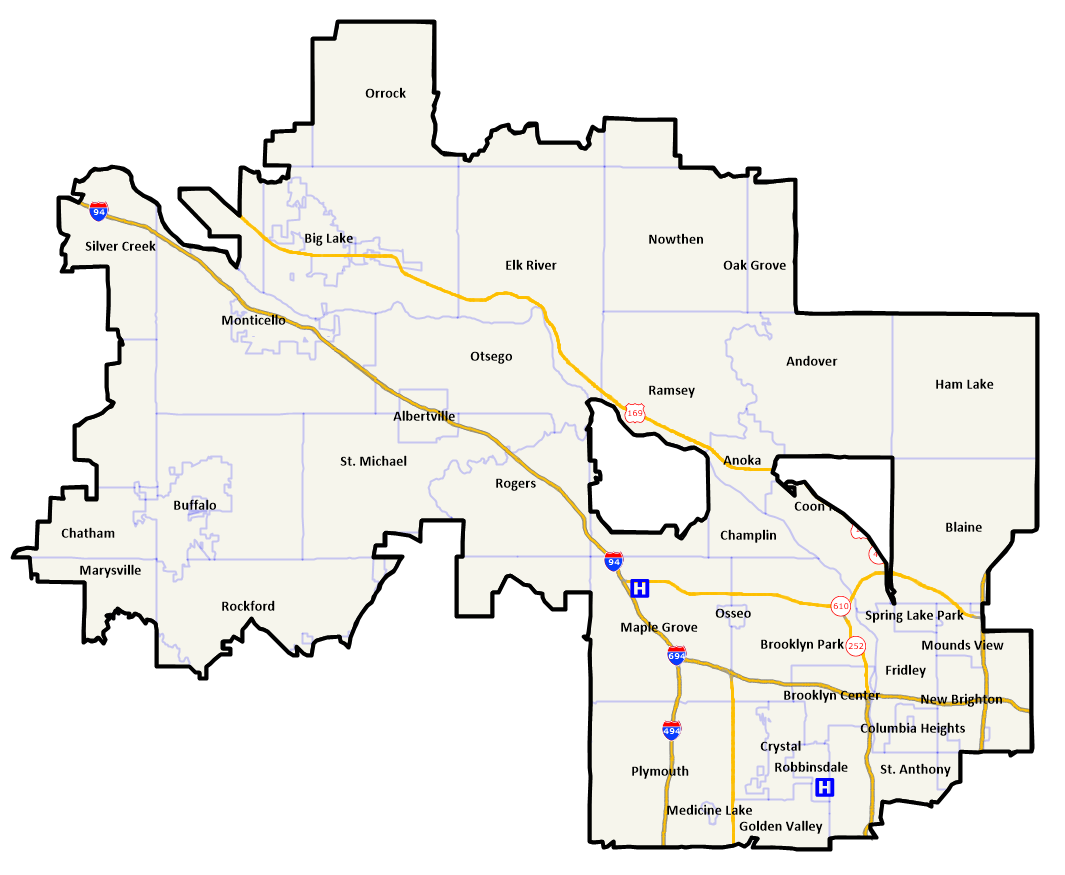
Our service area
The area selected for our Community Health Needs Assessment data analysis includes 75% of all patients admitted to North – Robbinsdale Hospital and North – Maple Grove Hospital in the year 2023.
It includes 31 ZIP codes, 34 cities and/or townships, and 7 school districts.
Past CHNAs and implementation plans
North – Maple Grove Hospital
2023
2022
2019
2016
2013
North – Robbinsdale Hospital
2023
2022
2019
2016
2013
Community Health Improvement Plan Update: 2023–2025
Over the past three years, North Memorial Health has actively implemented strategies outlined in the 2023–2025 Community Health Needs Assessment, focusing on two key priorities: racial disparities in health and life-impacting traumas.
North Memorial Health remains committed to advancing health equity and trauma-informed care through community collaboration, culturally responsive practices, and continuous learning. We are proud of the progress made and grateful to our partners and community members who make this work possible.