When Lauren Craft became pregnant with her third child, she knew early on that this pregnancy was unlike her other ones. “I was really scared,” says Craft. “Nothing felt right, and nothing felt the same.”
With her second child, Craft had complications, most severely a uterine rupture. Doctors were able to repair her uterus but knowing the risk that added to her pregnancy and the difference in how the pregnancy felt, she grew fearful.
Because she began to experience so much pain, at 19 weeks Craft’s OB-GYN doctor sent her to North Memorial Health Maternal-Fetal Medicine – Maple Grove to gather more detailed imaging. They saw that her lower uterine segment was minimal, meaning there wasn’t much to hold the baby in. Craft’s baby was going to come early, it was just a matter of when.

“I’m thankful they trusted that I didn’t feel right and identified what was wrong, but it created more fear in me,” says Craft. “I went home wondering if something was going to happen, knowing that if it did, I wouldn’t be able to get to the hospital fast enough.”
Between 19 and 26 weeks, Craft’s pain only worsened. Then, at 26 weeks and one day she had an ultrasound and her Maternal-Fetal Medicine doctor, Dr. Jessica Nyholm, told her that because of her pain, the state of her uterus and the distance she lived from the hospital, she’d have to stay at Maple Grove Hospital until her baby was born.
“The day I was admitted I cried because I was so relieved I was somewhere I knew I was safe,” says Craft. “If something happened, I was with all the right people. I was exactly where I needed to be.”
While Craft was in antepartum at the hospital, a neonatologist met with her to give her a tour of the Neonatal Intensive Care Unit (NICU) and prepare her for what to expect, knowing her baby would likely need to spend time there.
The doctors wanted Craft to be on bedrest until she hit 34 weeks, but at 28 weeks and four days they did what would be her last ultrasound. They could no longer see any uterine tissue — and told her that her baby was coming that day. She had been in the hospital for nearly three weeks.
“It was the realest day of my life because you don’t know what’s going to happen,” says Craft. “I was in a situation I couldn’t control and knew there wasn’t anything I could do to keep my baby in longer, love her anymore or to care for her any differently. My baby was coming, and I had to trust God and my doctors that she was going to be OK.”
On February 25, 2019, Craft’s daughter, Poppy, was born at 2 pounds, 10 ounces. Craft’s OB-GYN doctor, a specialist from Maternal-Fetal Medicine and a neonatologist from Minnesota Neonatal Physicians were all present in the delivery room, along with the other doctors and nurses.
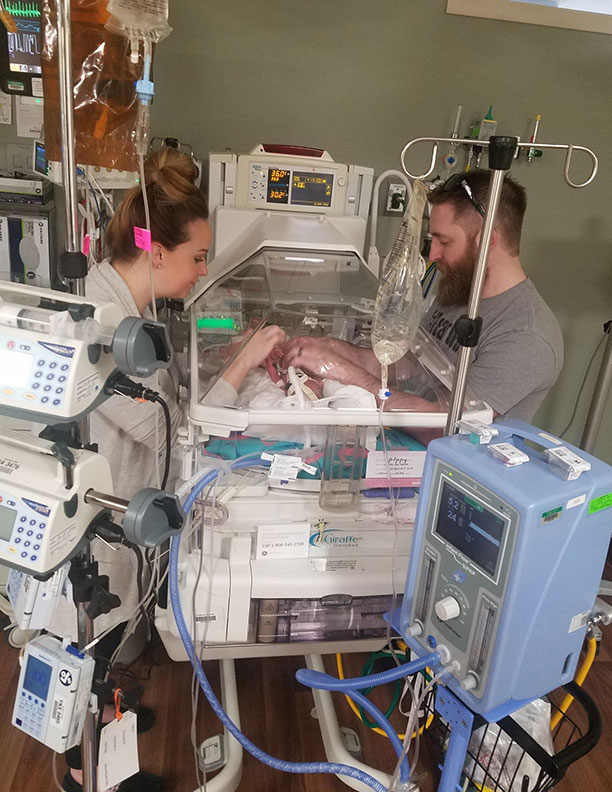
Four days after Poppy was born, Craft was discharged from the hospital, but Poppy wasn’t. She stayed in the Maple Grove Hospital NICU for 71 days. Craft came to visit Poppy every single day, staying for eight to 10 hours at a time.
“Poppy was born just at the end of the second trimester. From our standpoint, she wasn’t that tricky — she’s what we do,” says Dr. Jeanne Mrozek, member of Minnesota Neonatal Physicians and Medical Director of neonatal services at North Memorial Health. “What made her unique and stand out to all of us was the relationship we formed with Lauren.”
Over the course of her stay, Poppy was on a ventilator and received other respiratory support. She was hooked up to IVs, on and off a CPAP machine and had a blood transfusion.
When babies are born as early as Poppy, their organs are formed, but they’re still supposed to be on life support through the placenta. So, while her condition was appropriate for her gestational age, she needed external life support because she wasn’t getting it internally.
“You’re helpless as a parent,” says Craft. “But the team in the NICU made me feel safe because they created a relationship with us. I trusted them with Poppy; I trusted them to make the best decisions they possibly could for my baby. And they did an amazing job at including us.”
Craft could have chosen to stay in a boarding room at the hospital, but because she had two other kids she needed to care for, she drove back-and-forth each day to visit Poppy.
“Parents aren’t just welcome, they’re a necessary part of care,” says Dr. Mrozek. “And while the medical piece is a part of it, it’s also about finding out who they are and how this is affecting them. Some people are more private, and some are open. Lauren was open and we developed a strong relationship.”
Dr. Mrozek says as rewarding as it is to teach these families about the medicine they’re providing, they’re also there to support them emotionally. Because she knows when people go home, they never talk about how good their ventilator was, they talk about the nurses and doctors, how they were treated and how they were made to feel.
“When you go through something like this you feel every emotion — scared, afraid, alone, angry,” says Craft. “But when you have the support of the team, their conversation every day, their smiles and their laughs, you’re not just internalizing about your own situation. You leave happy knowing your baby is well cared for. There’s such a bond when you’re here for so long.”
Poppy was discharged one week prior to her due date. She’s doing well now, and the Craft family hasn’t had to bring her back into the hospital since.
“If I could explain my experience here from start to finish, if I could use one word, it’d be ‘amazing,’” says Craft. “There’s not one day I didn’t feel cared for or supported the whole time I was here. I felt safe and I felt like I was where I needed to be. And I know not all hospitals are like that and have staff like this one. Maple Grove Hospital made us feel like family.”
In addition to caring for families like the Craft’s, the NICU is consistently working to improve families’ experience and offer further support. Through the Maple Grove Hospital Fund, they’re able to provide comfort items and specialty equipment, as well as make efforts to optimize facilities for healing and family bonding.


